The gut is considered the center of our health – but what happens when the intestinal barrier becomes permeable? The so-called leaky gut syndrome, meaning “permeable intestine,” is increasingly being linked to a variety of chronic complaints. From digestive problems to skin diseases to chronic fatigue: the list of possible symptoms is long. But what exactly lies behind this phenomenon, and how can those affected restore their gut health? This guide provides well-founded answers to the most important questions about leaky gut syndrome.
What is Leaky Gut Syndrome?
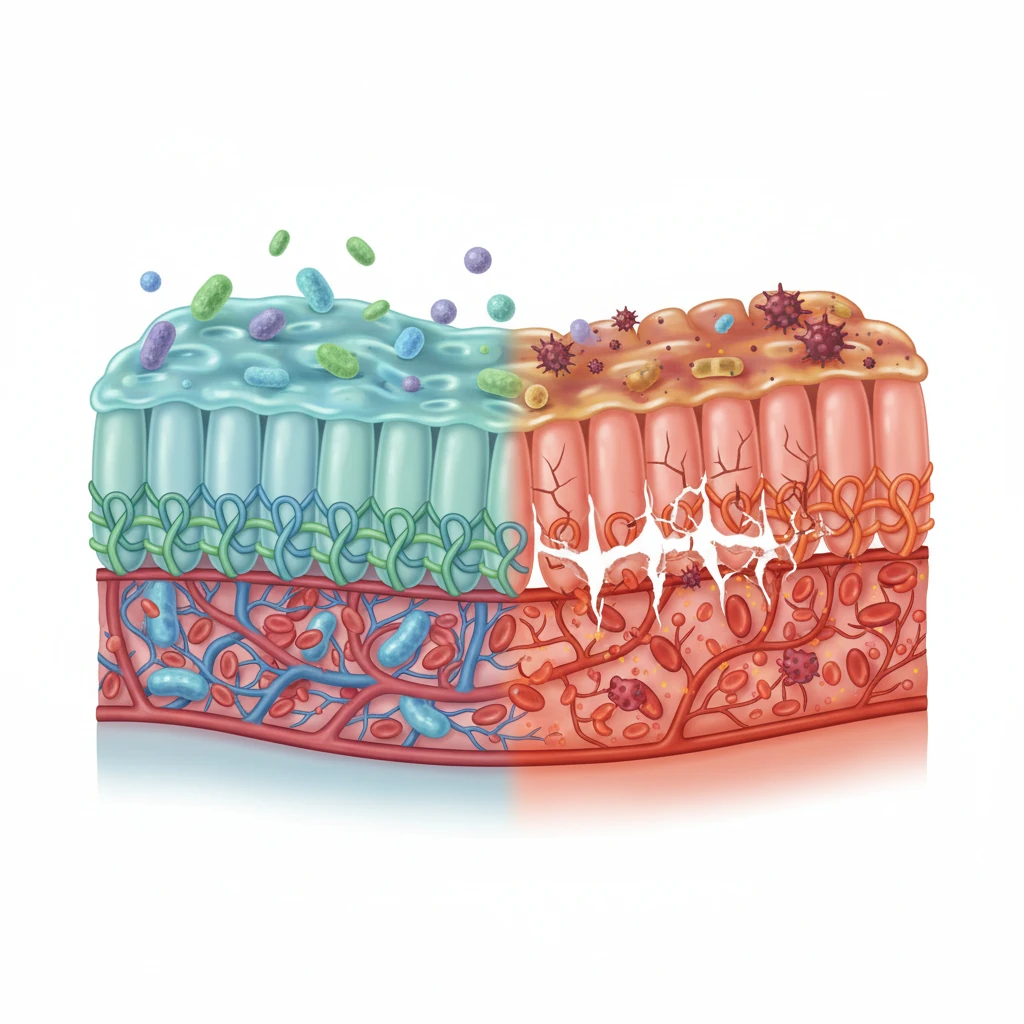
Leaky gut syndrome (increased intestinal permeability) describes a disorder of the intestinal barrier in which the permeability of the intestinal mucosa is increased. Normally, the intestinal wall functions like a selective filter: it allows nutrients, water, and electrolytes to pass through, but keeps out harmful substances, pathogens, and undigested food components.
The intestinal mucosa consists of a single cell layer, whose cells are held together by so-called tight junctions – tight connections. These tight junctions precisely regulate which molecules are allowed to pass the barrier. In leaky gut syndrome, these connections are weakened or damaged, allowing larger molecules, bacterial components, and toxic substances to enter the bloodstream.
The Intestinal Barrier in Detail
The intestinal barrier is a complex system of multiple protective layers. In addition to the epithelial cells with their tight junctions, it includes a mucus layer, antimicrobial peptides, and the gut-associated immune system (GALT). Approximately 70 percent of all immune cells are located in the gut, which underscores its central role for overall health.
An intact intestinal barrier is crucial for the body’s homeostasis. It not only prevents the entry of harmful substances but also enables communication between gut bacteria and the immune system – an essential process for the development and regulation of the immune response.
Causes of a Leaky Gut
The development of leaky gut syndrome is multifactorial. Various factors can impair the integrity of the intestinal barrier individually or in combination.
Dietary Factors
An unbalanced diet plays a central role in the development of a permeable intestinal wall. Particularly problematic are highly processed foods with many additives, sugar, and trans fats. These can promote inflammatory processes and negatively affect the gut microbiome. Excessive alcohol consumption also directly damages the intestinal mucosa and increases its permeability.
In celiac disease patients, gluten demonstrably leads to an opening of the tight junctions through the release of zonulin. This mechanism is also discussed in people with non-celiac gluten sensitivity, but the evidence here is less clear. Certain lectins from legumes and nightshade plants are also discussed. However, the evidence for relevant damage to the intestinal barrier in healthy people is limited. In cases of individual intolerance, an elimination trial may be useful.
Medications and Pollutants
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or diclofenac can damage the intestinal mucosa with prolonged use. Antibiotics, especially with frequent or improper use, also disrupt the microbial balance in the gut and can thus indirectly impair barrier function.
Proton pump inhibitors alter the pH value in the gastrointestinal tract and can influence the microbiome with long-term use and increase the risk of bacterial overgrowth, which can indirectly impair the intestinal barrier. Environmental toxins such as pesticides, heavy metals, and microplastics are also discussed as potential risk factors.
Stress and Lifestyle
Chronic stress has demonstrable negative effects on gut health. Via the gut-brain axis, stress influences intestinal motility, mucus production, and the permeability of the intestinal barrier. Stress hormones such as cortisol can weaken tight junctions and promote inflammatory processes.
Sleep deprivation, excessive exercise, and other physical stress factors can also burden the intestinal barrier. Lack of exercise, on the other hand, leads to slowed intestinal motility and can also be unfavorable.
Dysbiosis and Infections
An imbalance of the gut flora – the so-called dysbiosis – is both a cause and consequence of leaky gut. Pathogenic bacteria and parasites can directly damage the intestinal wall. Overgrowth with Candida albicans is also discussed as a possible factor, although the clinical relevance in individual cases is often difficult to assess. At the same time, in dysbiosis, important protective bacterial strains are missing that normally produce short-chain fatty acids and support barrier function.
Symptoms and Possible Secondary Diseases
The symptomatology of leaky gut syndrome is diverse and often nonspecific, which complicates diagnosis. Many sufferers experience various complaints for years without knowing the underlying cause.
Digestive Complaints
The most common symptoms include bloating, diarrhea, constipation, abdominal pain, and irritable bowel syndrome. These complaints arise from inflammatory processes in the intestinal mucosa and disrupted digestive function. Many patients also report food intolerances that develop over time.
Systemic Complaints
When bacterial components and undigested food particles enter the bloodstream through the weakened intestinal barrier, this activates the immune system. The resulting chronic inflammatory reaction can manifest throughout the entire body.
Typical systemic symptoms are chronic fatigue, lack of energy, concentration disorders, and “brain fog” – a feeling of mental fogginess. Skin problems such as acne, eczema, or psoriasis are also associated with a leaky gut. Joint pain, headaches, and increased susceptibility to infections can also occur.
Connection to Chronic Diseases
Research is intensively investigating possible connections between leaky gut and various chronic diseases. These include autoimmune diseases such as Hashimoto’s thyroiditis, rheumatoid arthritis, or multiple sclerosis. In allergies, asthma, inflammatory bowel diseases, depression, and metabolic syndrome, a disturbed intestinal barrier is also discussed as a possible contributing factor.
However, it is important to emphasize that a causal connection has not yet been clearly proven in many cases. It is often unclear whether increased intestinal permeability is the cause, consequence, or accompanying phenomenon of the respective disease. For some autoimmune diseases, there is evidence of increased permeability as a possible trigger factor, but research is not yet complete.
Diagnosis: How Can Leaky Gut Be Detected?
The diagnosis of leaky gut syndrome is not trivial. Increased intestinal permeability is a scientifically measurable phenomenon, but ‘leaky gut syndrome’ as an independent disease entity is controversial in conventional medicine and is not uniformly recognized as a diagnosis. Nevertheless, there are various examination options.
Laboratory Diagnostics
The zonulin test is one of the best-known markers. Zonulin is a protein that regulates tight junctions. Elevated zonulin levels in stool or blood can indicate increased intestinal permeability. However, the validity of this test is disputed among experts.
The lactulose-mannitol test functionally measures the permeability of the intestinal wall: after drinking a solution with these two sugars, it is measured how much of it is excreted in the urine. An abnormal ratio indicates a disturbed barrier function.
Other diagnostic approaches include stool examinations to analyze the microbiome, inflammatory markers such as CRP or calprotectin, as well as tests for food intolerances and nutrient deficiencies.
Clinical Assessment
Often the diagnosis is also made clinically based on symptoms and medical history. An experienced therapist can assess based on the overall picture whether leaky gut syndrome is likely and initiate appropriate therapy.
Treatment and Healing of the Intestinal Barrier
The therapy of leaky gut syndrome is based on a holistic approach that encompasses various levels. The goal is to eliminate the causes, reduce inflammation, and promote the regeneration of the intestinal mucosa.
Dietary Change
The basis of any successful treatment is a gut-friendly diet. This should be rich in whole, unprocessed foods. Particularly important are high-fiber foods such as vegetables, fruits, and whole grain products that nourish the microbiome.
Fermented foods such as sauerkraut, kimchi, kefir, or yogurt provide probiotic bacteria that positively influence the intestinal environment. Bone broth contains collagen, gelatin, and amino acids such as glycine and proline, which can theoretically support the intestinal mucosa. However, the scientific evidence for a therapeutic effect is limited.
On the other hand, sugar, highly processed foods, excessive gluten (at least temporarily), alcohol, and potentially irritating substances should be avoided. Some patients benefit from a therapeutically supervised elimination diet, in which potential trigger foods are initially omitted and later gradually reintroduced. This should ideally be done under the guidance of a nutrition professional to avoid nutrient deficiencies.
Probiotics and Prebiotics
Probiotics can help restore microbial balance. Particularly well-studied are strains such as Lactobacillus and Bifidobacterium. Prebiotics – indigestible fibers – serve as food for beneficial gut bacteria and should also be part of therapy.
Dietary Supplements
Various nutrients can support the regeneration of the intestinal mucosa. These include L-glutamine, an amino acid that is considered the most important energy source for intestinal cells, zinc, which is important for the integrity of tight junctions, as well as omega-3 fatty acids, which have anti-inflammatory effects.
Vitamin D, curcumin, and quercetin are also frequently recommended. Caution is advised with vitamin A, as it can be toxic in case of overdose – here supplementation should only occur after laboratory diagnostics. However, supplementation should always be coordinated with a therapist to avoid overdoses and interactions.
Stress Management and Lifestyle
Since stress is a significant factor for gut health, relaxation techniques such as meditation, yoga, breathing exercises, or progressive muscle relaxation should be integrated into daily life. Adequate sleep of generally seven to nine hours per night is essential for regeneration, although individual sleep needs may vary.
Moderate exercise promotes intestinal motility and has anti-inflammatory effects, while excessive exercise should be avoided. Social contacts and positive emotions also demonstrably influence the gut-brain axis.
Medical Treatment
In some cases, medical treatment may be necessary, for example, in proven infections with pathogenic germs or fungi. Optimizing existing medications or discontinuing unnecessary preparations should also be considered.
Prevention: Keeping the Gut Healthy Long-term
The best therapy is prevention. A gut-friendly lifestyle should be maintained permanently to prevent relapses and preserve gut health in the long term.
This includes a diverse, plant-based diet with many different fiber sources that promote the diversity of the microbiome. Careful use of medications, especially antibiotics and NSAIDs, protects the gut flora. Alcohol should only be consumed in moderation.
A mindful approach to stress, regular exercise, and adequate rest are just as important as avoiding smoking and reducing environmental toxins. Regular relaxation periods and time for social contacts also contribute to gut health.
Conclusion: Holistic Approach for a Healthy Gut
Leaky gut syndrome is a complex phenomenon that may be involved in the development of numerous chronic complaints. Although scientific research in this area has not yet conclusively answered all questions, studies and clinical experience clearly show that the integrity of the intestinal barrier is of central importance for overall health.
Treatment requires a holistic approach that includes diet, lifestyle, stress management, and possibly targeted supplementation. There is no universal solution – each patient requires an individual strategy tailored to their specific situation.
Anyone suffering from chronic, diffuse complaints for which no clear cause has been found should consider a leaky gut as a possible factor. Collaboration with an experienced doctor or therapist knowledgeable about gut health can help initiate the right diagnostic and therapeutic steps.
Ultimately, the examination of leaky gut syndrome shows once again how central the gut is to our health. Investing in a healthy gut flora and an intact intestinal barrier is an investment in quality of life and well-being – and may possibly be the key to solving many health problems.
Dieser Ratgeber dient ausschließlich zu Informationszwecken und ersetzt keine medizinische Beratung oder Diagnose. Bei anhaltenden Beschwerden konsultieren Sie bitte einen Arzt. Nahrungsergänzungsmittel und Heilpflanzen sollten nicht ohne Rücksprache mit einem Therapeuten eingenommen werden.